Picture the scene…
A 76 year old man presents to the ED with sudden onset back pain after trying to carry his luggage to the car. He’s keen to get some pain killers and leave to catch his plane as soon as he can…
Learning Objective
To learn about the management of the patient with back pain in the Emergency Department.
Task 1 – Read
Task 3 – Discuss
This part of the teaching session should be lead by an experienced clinician. The cases provided are merely examples and if possible the learners should be encouraged to discuss patients they have seen in their clinical practice.
Case 1 – A patient with back pain
A 38 year old presents with worsening back pain and shooting pains down her left leg.
1, What particular points will you ask about in the history?
It’s really important to ask about the red flag symptoms that might point towards a serious diagnosis such as cauda equina syndrome. In a patient of this age cancer (primary or metastatic) is less likely, but some simple screening questions such as unexplained weight loss, history of cancer and night pain are quick to ask and easy for the patient to answer.
If there is concern about cauda equina syndrome (and we must always rule out the serious diagnoses in the ED) ask about a history of difficulty emptying the bladder or bowels, pain and/or weakness in both legs and saddle-area anaesthesia over dermatomes S2, S3, S4 and S5 (a late sign).
2,What features would you look for on examination
There aren’t really any features of the clinical examination that can rule out cauda equina. The only feature that had a useful likelihood ratio in one series2,3 was urinary retention (LR+16.5). It always performed, but the PR examination isn’t really that discriminative at all.
3, What investigations would confirm the diagnosis?
Once cauda equina enters the differential diagnosis there is really only one investigation to rule out (or rule in) the diagnosis: MRI. Discuss with your facilitator how this would take place in your Trust.
Case 2 – A older patient with back pain
A 76 year old man presents to the Minors area of the ED with sudden onset back pain after trying to carry his luggage to the car. He’s keen to get some pain killers and leave to catch his plane as soon as he can. The pain was so bad that he fainted.
1, What are the key questions to ask in the history?
Firstly, don’t be distracted by this patient’s urge to leave or that he is in the Minors area. Stick to ruling out the “worst case scenario”. At this chap’s age his back pain really could be anything, including a ruptured AAA. Ask a detailed history about when the pain came on. Does he have a history of ischaemic heart disease or vascular disease?
2, What would you look for on a focussed examination?
Ask for (or measure yourself) a set of vital signs. Be even more suspicious if the patient is tachycardic or hypotensive (remember a fall in blood pressure may be relative and what’s “normal” for a 25 year old could be very low for a 76 year old). Gently feel his abdomen – is there a pulsatile mass?
3, What investigations would you request?
If AAA still hasn’t been ruled out, urgently talk to your senior Emergency Physician on shift. This patient needs a point of care ultrasound, which should be possible in most Emergency Departments
4, What would you do next?
If you haven’t already move the patient to the resuscitation room and ask your senior to join you at the bedside. You will manage this patient’s care together from now on.
Ensure the patient has adequate intravenous access and that a sample has been sent to the blood bank to type and cross match his blood. Give him pain relief, but be cautious so ask not to drop his blood pressure or make him feel sick (vomiting will increase his intraabdominal pressure and also make an anaesthetic more hazardous).
If this patient’s ultrasound confirms a AAA and the patient has other signs, especially hypotension, the surgical team may want to take him straight to theatre. If the ED team, anaesthetics and surgery think he is going to remain haemodynamically normal he may go for a CT scan prior to theatre for operative planning.
Case 3 – A young man with back pain after moving house
A 45 year old man (yes, that is young!) presents to the Minors area of the ED with sudden onset back pain that came on whilst lifting boxes into a removal van. He’s able to mobilise, but only just, The paracematol he took at home have “done nothing”.
1, What are the key questions to ask in the history?
The immediate thought is that this patient has musculoskeletal back and he probably has. BUT, we need to actively consider the serious diagnoses in all patients. A quick run through the “red flags” will help…
- neurological symptoms (especially altered sensation, disturbance of bladder and bowel function)
- weight loss
- known cancer (especially those which commonly metastatise to bone)
- fever or night sweats (consider infection especially TB)
- coagulopathy including patients on warfarin or DOACs
- immonosuppression
2, What would you look for on a focussed examination?
Double check that the patient’s neurology is normal in their legs.
Do a range of motion test of the patient to assess how restricting their pain is.
Not every patient with back pain needs a PR examination – only do this if you truly think there is a chance the patient may have neurological involvement.
3, What investigations would you request?
If you think this pain is muscular and there are no red flags the answer is none
4, What would you do next?
This patient needs analgesia and sensible advice about how to manage their pain.
They should start with paracetamol and a NSAID (if no contraindications) and if severe you may want to add in a opiod such as dihydrocodeine.
Benzodiazepines such as diazepam are often given as ‘muscle relaxants’ (sic) but if you remember the pharmocology they are really ‘patient relaxants (via GABA receptors). If the patient is acutely distressed by the pain these drugs may help to settle the situation down, but must only be used short term.
There are many excellent advice sheets available for patients. This one from Oxford is a good example.
Task 4 – Summary
In this session we have learned about the clinical assessment of the patient with headache in the Emergency Department
Consider these questions based on your learning today
1, What are the causes of back pain that we must rule out in the Emergency Department?
- Ruptured Abdominal Aortic Aneurysm
- Cauda Equina Syndrome
- Infection
- Malignancy
2, What are the “Red Flags” in the history that suggest a serious cause of back pain?
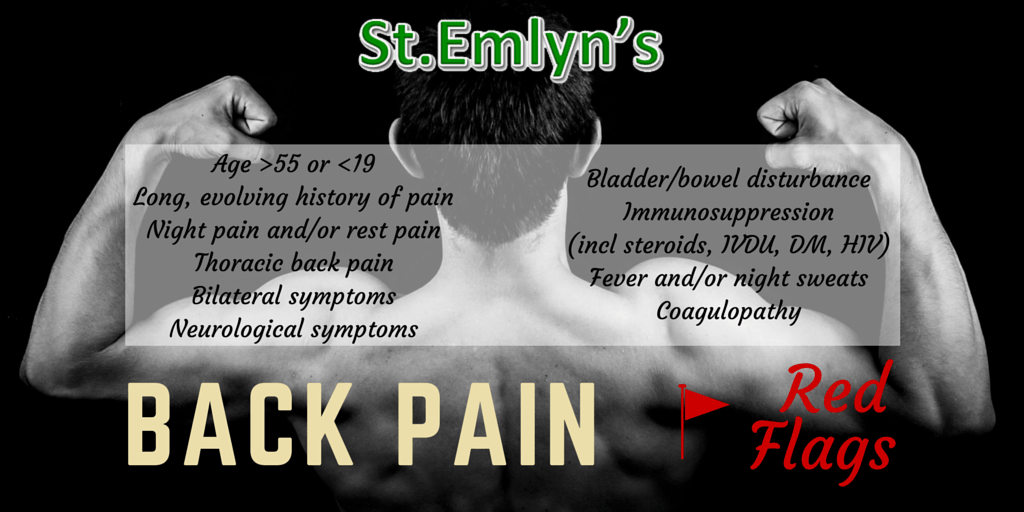
These “red flags” are important to consider in all patients with back pain. You will see lots of patients in your career with back pain and only a very few will have a sinister cause. You need to think of these every time to prevent you missing the infrequent serious diagnosis.
Task 5 – Reflect
In order to embed today’s learning further, reflect on what you have learnt and record in your portfolio whether it has had any impact (or is expected to have any impact) on your performance and practice.
Was this a topic that you were confident you knew already? Which parts were new to you? Were there elements that you will use on your next clinical shift.
Dscuss this session with your colleagues – were there people who missed it who you can share the highlights with?
References and Further Reading
- 1May N. Back to Basics – Back Pain in the ED. St Emlyn’s. 2015; published online Aug 20. https://www.stemlynsblog.org/back-to-basics-back-pain-in-the-ed/ (accessed June 6, 2020).
- 2Micks T. How useful is the physical examination in suspected cauda equina syndrome? Canadiem.Org. 2017; published online Aug 8. https://canadiem.org/how-useful-is-the-physical-examination-in-suspected-cauda-equina-syndrome/ (accessed June 6, 2020).
- 3Domen PM, Hofman PA, van Santbrink H, Weber WEJ. Predictive value of clinical characteristics in patients with suspected cauda equina syndrome. European Journal of Neurology 2009; : 416–9.