Picture the scene…
A paramedic crew pre-alert a patient who has had a 3 day history of black tarry stools and ‘coffee ground vomiting’…
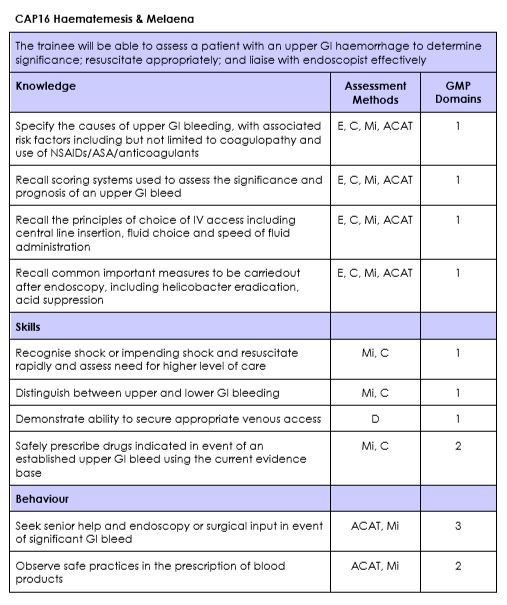
Learning Objective
To understand the presentation and immediate management of patients presenting to the ED with upper GI bleeding.
Task 1 – Knowledge
Read this St Emlyn’s blog post from Chris Gray.
Task 2 – Podcast
Listen to this podcast from the Resus Room.
Task 3 – Discuss
This part of the teaching session should be lead by an experienced clinican. The cases provided are merely examples and if possible the learners should be encouraged to discuss patients they have seen in their clinical practice.
Case 1 – A patient with dark stools
A 45 year old female presents to ED with a 48 hour history of dark tarry stools and a history of previous liver transplantation. Her initial Hb is 61 with a BP of 78/44 and a lactate of 7.1
1, How would you manage her initial resuscitation?
Manage in resus setting with high concentration oxygen and 2 wide bore IV cannulae
- Send bloods including FBC, U&E, LFTs, INR and cross match 6 units
- Check blood glucose (history of liver disease)
- Consider crystalloid while awaiting blood
- Manage massive bleeding as per local major haemorrhage protocols
- Transfuse those with Hb <7g/dL (<9g/dL if unstable Coronary artery disease)
- Platelets if count is <50 x 109/L and actively bleeding
- FFP in actively bleeding patient with INR >1.5
- Reverse oral anticoagulation in actively bleeding patients (Involve haematology)
- No evidence for TXA yet, (HALT-IT)
- Urgent referral: Involve endoscopist and critical care team
2, What are the differences in the management of variceal vs non-variceal bleeding?
Variceal bleed
- Vasopressins: Terlipressin causes arterial vasoconstriction, reducing portal venous pressure but carries a risk of end organ ischaemia. Can reduce blood loss from actively bleeding varices and results in a relative risk reduction in mortality2
- Somatostatins: Octretide causes a relaxation in vascular smooth muscle and reduces portal venous pressure. Safer in patients with ischaemic heart disease but more difficult to give
- IV antibiotics: 20% of cirrhotic patients with variceal bleeding will develop a bacterial infection within 48 hours3
- Massive uncontrollable variceal haemorrhage may require a sengstaken tube
Non-variceal bleed
- PPIs (Omeprazole/Pantoprazole) are widely used. Theoretical improvement in clot stability and reduction in bleeding. Evidence of reduced risk of re-bleeding if used post endoscopy. No reduction in mortality. Not currently recommended for routine use in ED by NICE4. May be of benefit if endoscopy is delayed
3, When should the patient go for endoscopy?
- Immediately after resuscitation for unstable patients. Requires clear communication and coordination with endoscopist and constant re-assessment of patient
- Likely to require theatre rather than endoscopy suite
- Within 24 hours of admission for all other patients
Case 2 – A patient with coffee ground vomiting
A 28 year old male presents to ED with coffee ground vomiting. He has been using ibuprofen for the last 2 weeks following a knee injury.
1, What are the common causes of UGI bleeds?
60,000 admissions per year in the UK
84-172 per 100000 population with mortality of 10%4
| Peptic ulcer disease 30% | Oesophagitis 10% |
| No diagnosis/other 20% | Varicies 10% |
| Mallory Weiss tear 15% | Vascular lesion 4% |
| Erosion 10% | Malignancy 1% |
2, How do we risk assess patients with suspected UGI bleeds?
Remember to take a thorough history. Some patients will present with dizziness or collapse without obvious bleeding. Remember PR exam
Variceal bleeding carries the highest mortality (50% in hospital mortality) with around 30% risk of re-bleeding5
Look for evidence of liver disease such as jaundice, ascites and encephalopathy
Various risk scores are in use such as Rockall and Glasgow-Blatchford. Glasgow-Blatchford is recommended for use pre-endoscopy in ED by both NICE and RCEM
3, How do we manage “low risk” patients?
Follow local protocol but be aware of responsibility to arrange onward care or referral from secondary care.
Low risk (Blatchford 0) patients with suspected upper GI bleeding may be appropriate for ambulatory management, but this should be supported by robust governance and locally agreed pathways.
Follow up of these patients should not be handed back to primary care routinely, unless as part of a local agreement.
Task 4 – Summary
In this session we have discussed the variable presentations of suspected upper GI bleeding. We have covered the management of the haemodynamically unstable patient and what parameters we should use to guide resuscitation. We have also covered the stable patient, risk assessment and differentiating between variceal and non-variceal bleeding.
Task 5 – Reflect
In order to embed today’s learning further, reflect on what you have learnt and record in your portfolio whether it has had any impact (or is expected to have any impact) on your performance and practice.
Was this a topic that you were confident you knew already? Which parts were new to you? Were there elements that you will use on your next clinical shift.
Dscuss this session with your colleagues – were there people who missed it who you can share the highlights with?
References and Further Reading
- 1Skinner J. Upper gastrointestinal haemorrhage. RCEM Learning. 2018; published online Jan 13. https://www.rcemlearning.co.uk/reference/upper-gastrointestinal-haemorrhage/#1571744062306-b0b0d3c9-0a4f (accessed June 10, 2020).
- 2Ioannou GN, Doust J, Rockey DC. Terlipressin for acute esophageal variceal hemorrhage. Cochrane Database of Systematic Reviews 2003; published online Jan 20. DOI:10.1002/14651858.cd002147.
- 3Lee YY. Role of prophylactic antibiotics in cirrhotic patients with variceal bleeding. WJG 2014; : 1790.
- 4NICE Guidance on Upper GI Bleeding (CG141). NICE. 2016; published online Aug 25. https://www.nice.org.uk/guidance/cg141/chapter/1-guidance (accessed June 10, 2020).
- 5Vreeburg EM, Terwee CB, Snel P, et al. Validation of the Rockall risk scoring system in upper gastrointestinal bleeding. Gut 1999; : 331–5.