Picture the scene…
A patient arrive in the Resus area of the ED. The consultant is busy with four Major Trauma patients in the other bays and asks you “Please can you see the new patient? Just make sure they don’t die”…
Learning Objective
To learn about the management of the patient with shortness of breath in the Emergency Department.
Task 1 – Read
Task 3 – Discuss
This part of the teaching session should be lead by an experienced clinician. The cases provided are merely examples and if possible the learners should be encouraged to discuss patients they have seen in their clinical practice.
Case 1 – A patient with shortness of breath
A 65 year old woman arrives into Resus via blue light ambulance at the end of your night shift with acute shortness of breath. She was woken from sleep and “felt like I was drowning”.
1, What are your first actions?
Firstly, remind yourself that this patient needs you! You are likely very tired and keen to go home, but this lady cannot wait for the day team to come on.
She is acutely unwell and needs immediate therapy. It is one of those times where you will need to start some treatment, whilst getting the key aspects of the history.
If she has low oxygen saturations, put on high flow oxygen (although she may be a smoker and have a history of COPD now is not a time to withhold giving her enough oxygen.
Get a set of vital signs and ask the nurses to perform an ECG. When the cannula is inserted ask for a venous blood gas.
2, The vital signs are Pulse: 120 reg; BP 180/90; Sats 95% (on oxygen); Respiratory rate 20/min; Temperature 37.2oC. What do you think the most likely diagnosis is in this patient?
Always think about our five life threatening causes of shortness of breath: in this case acute left ventricular failure seems most likely. She could have COPD, but the time of time of presentation and high blood pressure are highly suggestive of a sympathetic driven response to acute LVF2.
3, What investigations would confirm the diagnosis?
A chest Xray may be helpful, but in most cases the diagnosis is a clinical one. An ECG will show if there is any ongoing ischaemia (or if this is related to an acute myocardial infarction). You may be able to get an echocardiogram, but in the acute phase it may be hard to interpret.
4, What treatment would you give?
Supplemental oxygen and a venodilator (to reduce the systemic vascular resistance and help the heart to pump more effectively) are the mainstays of treatment. Glyceryl Trinitrate (GTN) can be given in many forms – you could start by given two puffs under her tongue, whilst you set up an infusion. This can then be titrated to effect – remember not to reduce her blood pressure too low (her usual may be slightly higher than we’d like). If her venous blood gas shows she is in type 2 respiratory failure then non invasive ventilation may be useful. You should involve one of your seniors early in this lady’s management
Case 2 – A young patient with shortness of breath
A 25 year old attends the ED with sudden onset shortness of breath. He is usually fit and well, and is a keen basketball player. He doesn’t smoke or take any medications.
1, What are the key questions to ask in the history?
When we see “young, fit” patients in the ED it is all too easy to dismiss their presentation as trivial, but remember – most people really do not want to be in an Emergency Department. When we think of the five life threatening causes of breathlessness that we must rule out left ventricular failure seems unlikely; he has no history of asthma; no symptoms of pneumonia and no obvious risk factors for PE. That leaves spontaneous pneumothorax as the only potentially serious diagnosis (and his love of basketball suggests he may be tall and thin….)
2, What would you look for on a focussed examination?
The “ATLS” version of (tension) pneumothorax is really difficult to elicit and only happens very late (tracheal deviation etc). Much more likely are simple things like a fast respiratory rate and decreased saturations. You may be able to notice quieter breath sounds on the affected side.
3, Which investigations would you request?
There is really no need for blood tests in this patient. The diagnosis is likely to be made on a chest radiograph, or using bedside ultrasound.
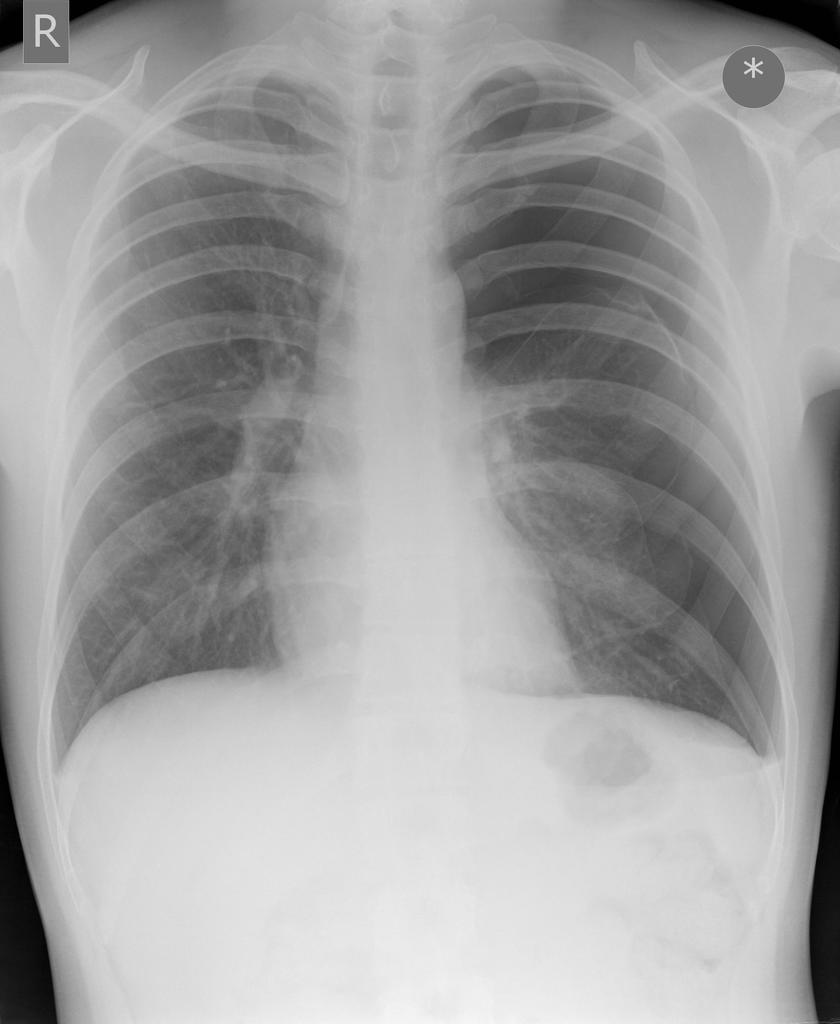
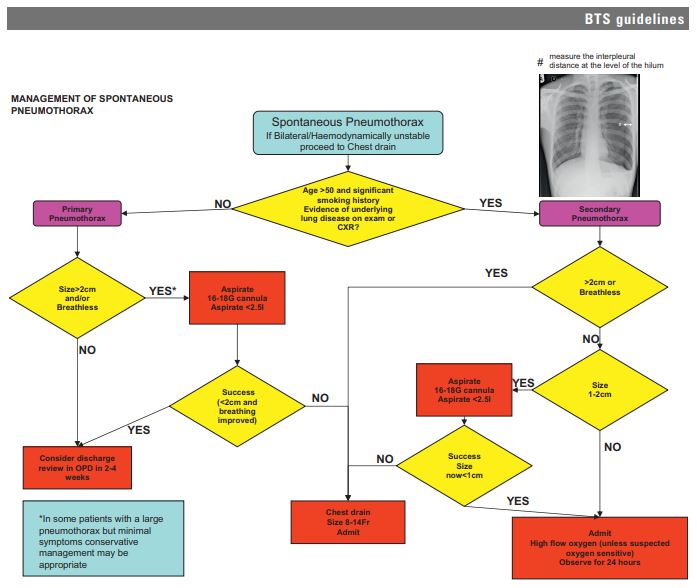
As with any investigation where you have two sides to compare look and see if the left and right look similar. Here there is a large left sided pneumothorax.
Task 4 – Summary
In this session we have learned about the clinical assessment of the patient with shortness of breath in the Emergency Department
Consider these questions based on your learning today
1, What are the five life threatening causes of shortness of breath that we must exclude?
- Acute left ventricular failure
- Asthma/COPD
- Pulmonary Embolism
- Pneumothorax
- Pneumonia
2, True or False – Oxygen should never be given to a hypoxic patient in case they are a “CO2 retainer”
FALSE. NOOOOO!!!!! Hypoxia kills. Oxygen should be used in the patient with shortness of breath and the patient monitored closely.
Task 5 – Reflect
In order to embed today’s learning further, reflect on what you have learnt and record in your portfolio whether it has had any impact (or is expected to have any impact) on your performance and practice.
Was this a topic that you were confident you knew already? Which parts were new to you? Were there elements that you will use on your next clinical shift.
Dscuss this session with your colleagues – were there people who missed it who you can share the highlights with?
References and Further Reading
- 1May N. An Introduction to the Breathless Patient in the ED. St Emlyns. 2014; published online Aug 3. https://www.stemlynsblog.org/induction-breathless/ (accessed June 6, 2020).
- 2Weingart S. EMCrit Podcast 1. EmCrit. 2009; published online April 25. https://emcrit.org/emcrit/scape/ (accessed June 6, 2020).
- 3Jones J. Spontaneous Pneumothorax. Radiopaedia. https://radiopaedia.org/cases/spontaneous-pneumothorax (accessed June 6, 2020).
- 4MacDuff A, Arnold A, Harvey J. Management of spontaneous pneumothorax: British Thoracic Society pleural disease guideline 2010. Thorax 2010; : ii18–31.