Picture the scene…
You see a patient who has had a clash of heads whilst playing football. They think they might have blacked out…
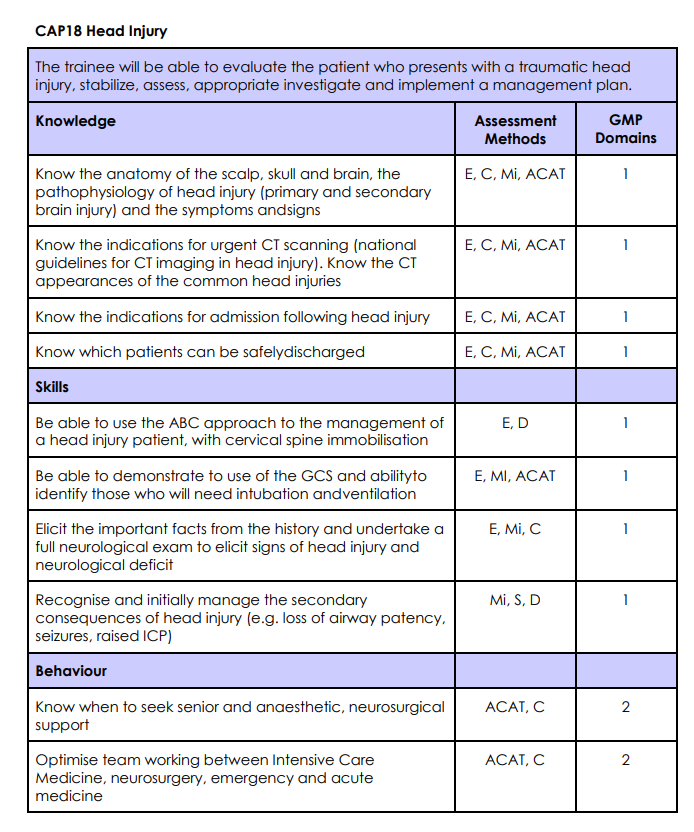
Learning Objective
In this session we will cover the anatomy and physiology and clinical management of patients with head injury.
Task 1 – Listen
Listen to this comprehensive epsiode of Crackcast covering everything you need to know about Head Injury. There’s a lot of information here – try to make notes as you go along to maintain focus. Everything they discuss is also on their excellent website.
Task 2 – Read
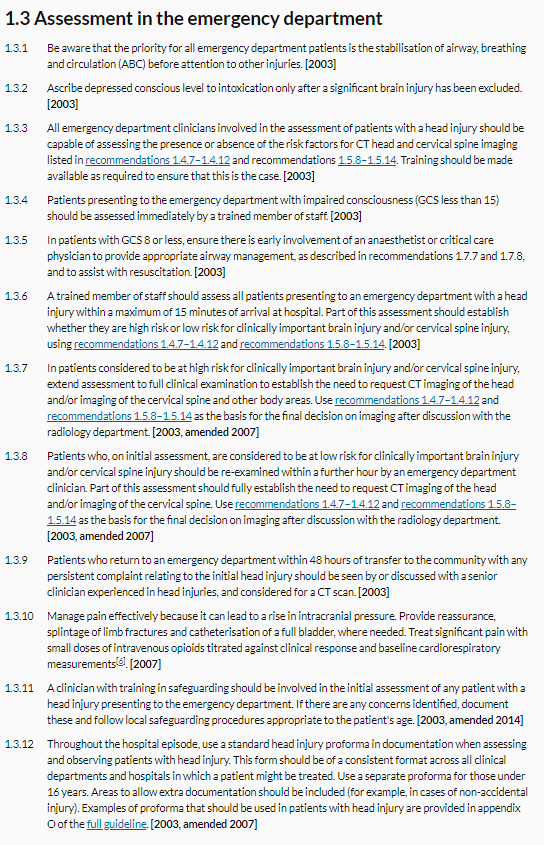
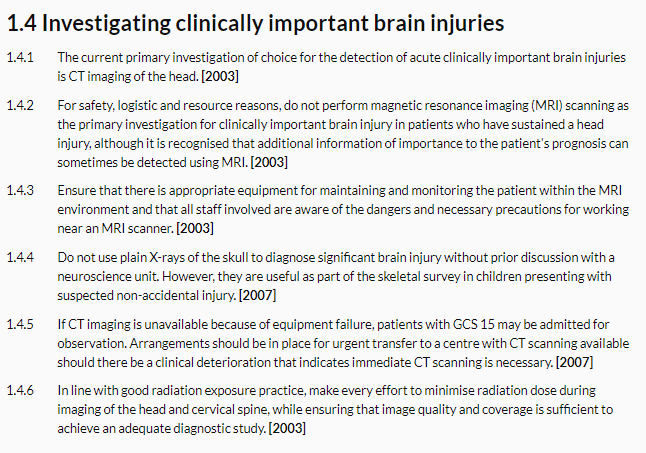
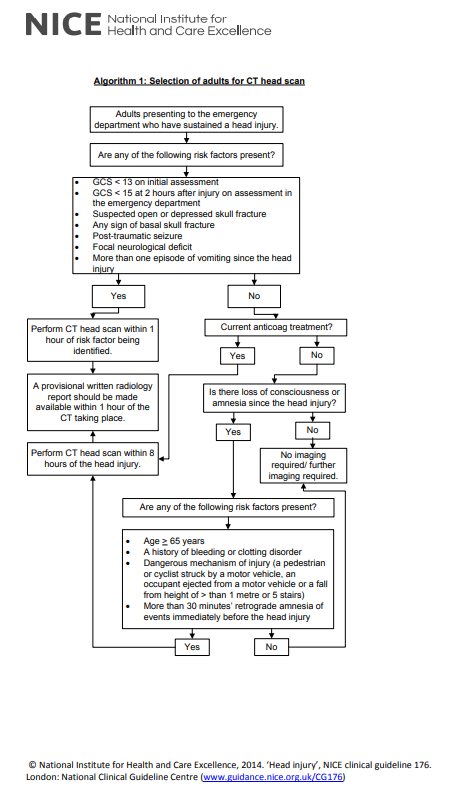
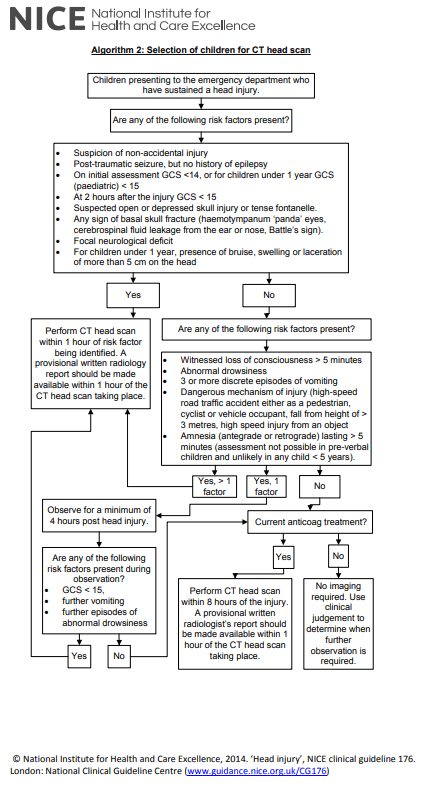
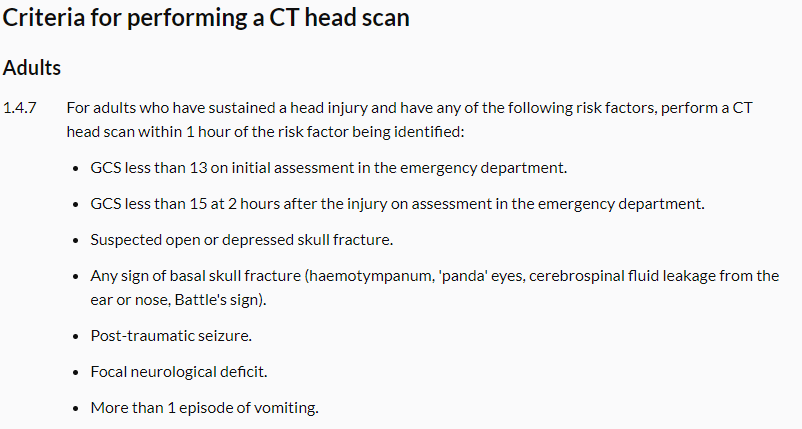
Read these excerpts from the NICE Head Injury Guideline. Click on each to view them full screen in a new window. If you have extra time there is an excellent interactive flowchart here.
Task 3 – Discuss
This part of the teaching session should be lead by an experienced clinican. The cases provided are merely examples and if possible the learners should be encouraged to discuss patients they have seen in their clinical practice.
Case 1 – A patient who fell from a ladder
A 56 year old previously fit and well man is brought to hospital by the paramedics after falling 6 feet off a ladder. He seems confused when he talks, will reach for your hand when you try to cannulate him and is opening his eyes to voice. There is a developing bruise on his head, but no other injuries reported.
1, What are you first actions when assessing this patient?
As with any patient who has had a traumatic injury you should first assess their ‘ABC’: Airway, Breathing and Circulation.
This patient is talking (so his airway is clear) and you akthough there are no other injuries reported you should assess the breathing and criculation. In this patient’s case there is no abnormality.
Before going any further consider if the patient needs any analgesia: we have a duty to ensure that our patients have as little pain as possible (plus if there is a significant head injury then pain can cause a rise in intracranial pressure).
2, What is this patient’s Glasgow Coma Score (GCS)?
The Glasgow Coma Score is made up of three parts: Eyes (scored out of four); Verbal (scored out of 5) and Motor (scored out of 6).Therefore the highest score a patient can get is 15. As the lowest score for each is one the lowest total score possible is 3.
Eye response (E)
There are four grades starting with the most severe:
- No opening of the eyes
- Eye opening in response to pain stimulus.
- Eye opening to speech. Not to be confused with the awakening of a sleeping person; such people receive a score of 4, not 3.
- Eyes opening spontaneously
Verbal response (V)
There are five grades starting with the most severe:
- No verbal response
- Incomprehensible sounds. Moaning but no words.
- Inappropriate words. Random or exclamatory articulated speech, but no conversational exchange. Speaks words but no sentences.
- Confused. The person responds to questions coherently but there is some disorientation and confusion.
- Oriented. Person responds coherently and appropriately to questions such as the person’s name and age, where they are and why, the year, month, etc.
Motor response (M)
There are six grades:
- No motor response
- Decerebrate posturing accentuated by pain (extensor response: adduction of arm, internal rotation of shoulder, pronation of forearm and extension at elbow, flexion of wrist and fingers, leg extension, plantarflexion of foot)
- Decorticate posturing accentuated by pain (flexor response: internal rotation of shoulder, flexion of forearm and wrist with clenched fist, leg extension, plantarflexion of foot)
- Withdrawal from pain
- Localizes to pain (purposeful movements towards painful stimuli)
- Obeys commands (the person does simple things as asked)
Our patient confused (V=4), will localise to pain (M=5), and is opening his eyes to voice (E=3), so his GCS is 12/15
3, Would you request a CT scan?
Yes! This patient fulfills one of the first criteria, which is a GCS of less than 13 on initial assessment in the Emergency Department.
Case 2 – A footballer after a clash of heads
A 21 year old female presents with her team physio after a head injury after a clash of heads during a football game. She went to head a ball and headed one of her opponents instead. She did not lose consiousness and has not vomited. She has a mild headache.
1, Does this patient require a CT scan?
From the description it doesn’t appear that she meets any of the criteria for CT brain scan.
2, The team Physio tells you that she got all of Maddock’s questions right. Is this a good thing?
Maddocks’ questions are part of a pitchside screening test that can be used for concussion.
When asking the Maddocks’ questions then the questions should be preceded with the preface: “I am going to ask you a few questions, please listen carefully and give your best effort.”
- What venue are we at today?
- Which half is it now?
- Who scored last in this match?
- What did you play last week?
- Did your team win the last game?
It is a relatively sensitive, but not specific test (players who answer all the questions correctly are unlikely to have concussion, wheras those who fail to answer one or two questions correctly may not have concussion).
The SCAT5 is the comprehensive assessment that incoporates the Maddocks’ questions, with the modified World Rugby Head Injury Assessment (HIA01) screening tool an example of a shortened version that can be used during a game.
3, What should the patient do over the next few days?
The Headway discharge advice sheet is excellent. It lists some important “Dos and Donts”
Do…
- DO make sure you stay within reach of a telephone and medical help in the next few days
- DO have plenty of rest and avoid stressful situations
- DO show this factsheet to a friend or family member who can keep an eye on your condition
- DO take painkillers such as paracetamol for headaches
Don’t…
- DON’T stay at home alone for 48 hours after leaving hospital
- DON’T drink alcohol until you feel better
- DON’T take aspirin or sleeping tablets without consulting a doctor
- DON’T return to work until you feel ready
- DON’T play or train for any contact sport for at least three weeks without consulting your doctor
- DON’T return to driving until you feel you have recovered. If in doubt consult your doctor.
Patients can suffer some symptoms for weeks or even months after an injury:
- Headaches
- Irritability
- Feelings of dizziness
- Restlessness
- Nausea
- Impulsivity and self-control problems
- Sensitivity to light or noise
- Difficulties with concentration
- Sexual difficulties
- Feeling depressed, tearful or anxious
- Sleep disturbance
- Fatigue
- Memory problems
- Difficulties thinking and problem-solving
4, What advice can you give to help lesson the effects of concussion?
The ‘post concussion syndrome’ is a very real and potentially disabling spectrum of symptoms that can be cognitive, emotional, physical or a mixture of all of these.
Again, Headway have produced an excellent booklet describing all of these symptoms and some strategies to manage them, but they can be summed up by the phrase ‘be kind to yourself’. You should remind the patient to not rush their recovery and ask for help from friends if they need it.
Task 4 – Summary
In this session, we have covered the diagnosis and initial management of head injury, from the very severe to relatively mild. We have discussed the indications for a CT scan and the suggested assessment of the patient with concussion.
Task 5 – Reflect
In order to embed today’s learning further, reflect on what you have learnt and record in your portfolio whether it has had any impact (or is expected to have any impact) on your performance and practice.
Was this a topic that you were confident you knew already? Which parts were new to you? Were there elements that you will use on your next clinical shift.
Dscuss this session with your colleagues – were there people who missed it who you can share the highlights with?
References and Further Reading
- The Assessment of Orientation Following Concussion in Athletes Maddocks D, Dicker G, Saling M. Clinical Journal of Sport Medicine (1995)
- The Sport Concussion Assessment Tool 5th Edition (SCAT5) Echemendia R, Meeuwisse W, McCrory P. Br J Sports Med (2017)